
- POPSUGAR Australia
- Fitness
- ‘Competitive Drive’ Is the Least of Our Problems When It Comes to Reproductive Health
‘Competitive Drive’ Is the Least of Our Problems When It Comes to Reproductive Health

Last week, the Sydney Morning Herald published an article titled: “Is the Pill Blunting Women’s Drive to Achieve?” The article referenced a recent University of Melbourne study, which indicated that during a “normal” cycle, people who have periods experience an increase in a motivational drive around the time of ovulation.
“Those who used hormonal contraceptives had their desire to achieve ‘flattened’ over the course of a month,” reported SMH. But that wasn’t quite true. While the study indicated that those not on contraception experienced a motivational increase once a month before menstruation, during the rest of the month their motivation levels were exactly the same as those on birth control.
SMH summarised: “Until now, no one has known much about the psychological impact of the pill on more than 100 million women each day,” but is that correct?
When the Pill Goes Viral
It’s not entirely true to say we don’t know much about the psychological impact of hormonal contraceptives, but it is a relatively narrow field of study. Interest in the psychological impacts of the pill waxes, wanes, and occasionally blows up.
One of the most popular studies is from 2008, when the Royal Society reported that people who were taking the pill found that their attraction to their partner vanished once they were off it.
Time picked it up in 2014, and it was circulated by The Guardian, Bustle, and numerous blogs. Vice revived the study in 2019 when it again went viral, featured in The Guardian (again), NY Post and name-checked in personal essays in several local publications.
While follow-up research has not found evidence to support the Royal Societies’ initial findings, the study remains immensely popular with journalists and ex-husbands.
Similarly, the “flattening competitive drive” study has now been republished by 10 different publications across Australia and the UK since the SMH story.
Are These Studies Problematic?

Dr Lucy France has worked in General Practice for over 30 years, and specialises in reproductive health and family planning.
France says that while there’s nothing inherently problematic about these studies, the reporting around them can be.
“You have to be so careful reporting these stories because a lot of people are not trained in analysing scientific reports,” France said. With flimsy reporting, she explained, there is a risk that the results of any scientific trial could be taken “as gospel” by the general public, even when they are in their early phases.
Related: The 4 Phases of Your Period Are Important to Understand — Here’s Why
In the University of Melbourne study reported on by SMH, they analysed 4,000 diary entries from the participants. It may sound like a lot, but for a medical trial, it’s actually quite limited in both length and depth, France explained.
“It’s a very short trial,” she said. “Forty days is one cycle, and being self-reported there are many holes in the methodology.”
This is not to say that research in this area is to be scoffed at, the issue for France is that it exists in a vacuum.
“I would love to see more research into behaviour on the pill, to see what is going on,” France said, “but that would involve many, randomly selected people over a far longer period of time.”
So, Does the Pill Impact Motivation?
We can’t move on without answering the burning question first. Could the pill be preventing you from #slayingit at your job?
It’s complicated.
“In a natural cycle, you will experience a surge of oestrogen before you ovulate, which research can suggest increases libido,” France said. She explained: “It’s a human survival mechanism — you want to have sex when you’re ovulating.”
Some research connects high libido with self-confidence, but it’s not understood which one is responsible for the other. France said that it’s possible a surge in oestrogen could correlate with higher energy, decisiveness and self-confidence, but that comes with a big caveat.
The research study and its conclusions are geared towards what France describes as “a woman or person with a ‘textbook’ cycle,” and many people just don’t fit the bill.
“There are many reasons people take the pill, not just for contraception,” she explained. These include acne, polycystic ovaries, premenstrual dysphoric disorder, endometriosis and quite simply terrible pain.
The study also excludes the experiences of trans men and non-binary people, for whom the experience of menstruation can be distressing in and of itself.

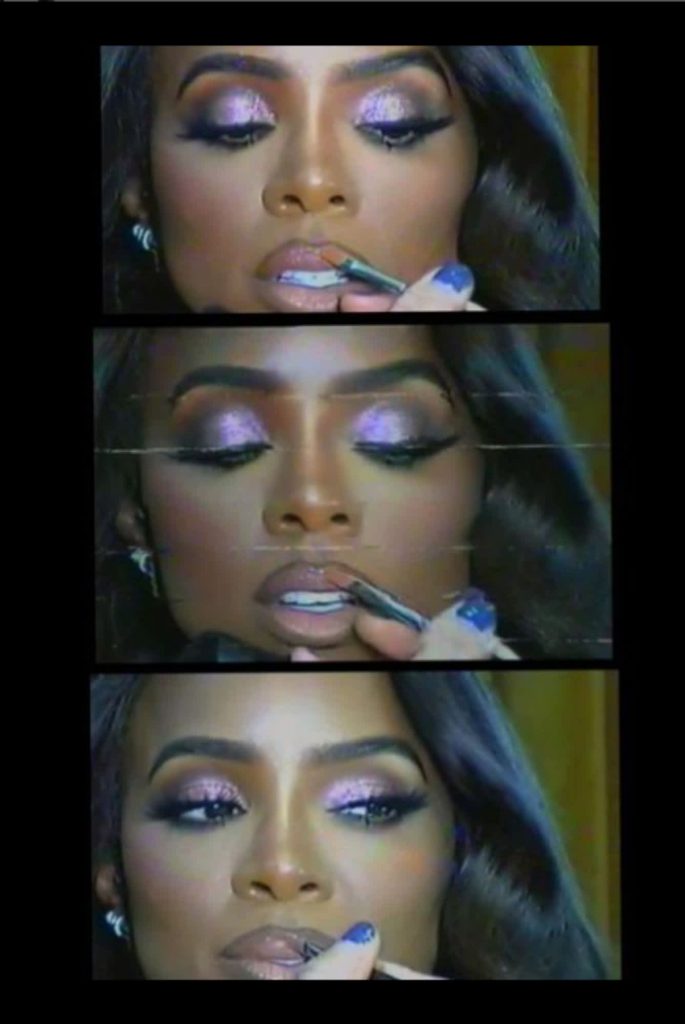
Nobody experiencing these pre-menstrual symptoms is likely to be blasting Kelly Rowland’s “Motivation” before heading to work to negotiate a pay rise.
Related: Worried You’ll Gain Weight on the Pill? It’s Not as Much a Concern as You Think
Then, there are also the productivity-reducing emotional impacts of an unwanted or unplanned pregnancy, which is something 50% of people who can get pregnant will experience in their lifetime.
Just earlier this month, another SMH article reported that many young people were ditching the pill, fuelled by concerns around physical and mental wellbeing, and opting for “natural” and unreliable contraception alternatives including withdrawal during sex and fertility timer apps.
Dr France said that unplanned pregnancies are one of the first issues she raises with patients who are looking to switch from the pill to natural contraception, and even physical forms of contraception, which are slightly less reliable than the pill.
“I will always explore the risk of pregnancy, and how concerned they would be if they fell pregnant,” she said. For some people, who are in a stable relationship or already contemplating a child, this risk might be nominal, for others, it could be devastating.
What We’re Not Talking About When We Talk About Reproductive Health
Is workplace productivity the first thing on people’s minds when managing their reproductive health?
After speaking to a handful of individuals who have been on and off the contraceptive pill over the years, there were some consistent themes, but none of them were work-related.
The majority of women we spoke to first started taking the pill in their early to mid-teens. While some used it as a form of contraception, it was more commonly used to control period pain or manage acne. The most common complaints? Mood, weight gain, and more than anything, frustration that the pill was suggested as their only option.
Related: The 4 Phases of Your Period Are Important to Understand — Here’s Why
Sarah* started the pill at 16, and over a period of 10 years tried six different brands. She struggled with moodiness, acne and migraines throughout, but felt unsupported in trialling different forms of contraception.
“Throughout this period I felt like I was the problem, not the pill,” she told POPSUGAR Australia.
For some, while the pill was effective, reporting on the pill was frightening. “I’ll always be grateful to my mum and GP,” Angela said of the decision to turn to the pill as an acne management strategy at 15.
“It meant that for eight years I had a reprieve from literally, and figuratively, picking myself apart,” she explained. At 23, the pill Angela was taking was banned in France after causing four deaths. While her GP assured her the likelihood of this complication was extremely low, she was spooked and stopped taking the pill. Her acne returned aggressively and is now managed with Roaccutane.
“For me, the pill didn’t mess with my mental health and the mental health ramifications of not being on it and battling with my skin have had a far worse effect.” Ultimately though, Angela feels women shouldn’t have to weigh up these risks.

Why Don’t We Have Better Alternatives?
For Dr France, the most pressing issue with reproductive healthcare is a lack of research and a lack of investment.
“Women are missing in action in major medical research,” she said, and it’s not just limited to reproductive health.
In the 60s and 70s, she told POPSUGAR Australia, all cardiovascular research was done on men. According to a study undertaken by Berkley, the University of California and the University of Chicago, women are twice as likely as men to suffer adverse reactions to medications, and more than 90% of women experienced worse side effects from medications.
Related: Why Isn’t There More Research on Menstruation in Sports? Dina Asher-Smith Calls For Action
This is because clinical trials for drugs, from antidepressants to cardiovascular treatments, anti-seizure medications and analgesics are undertaken on men.
Conditions that don’t affect cisgender men receive even less attention. France said that at the other end of the fertility spectrum, there is also a total blind spot in medical research when it comes to menopause, which can severely impact quality of life.
“For example, women gain weight during menopause, but we don’t actually understand the mechanism,” she said. Instead, like women who are offered the pill to manage menstrual complications, women experiencing menopause-related weight gain are told to make lifestyle changes like increased exercise and dietary restrictions.
For France, while the University of Melbourne study is limited, she would welcome many more.
“Bring it on, the more the merrier!” she said.
Meanwhile, if you’re worried about something you see online? A good GP will help you make a decision.
“Since the 60s when the pill was introduced, the hormonal dose has gone down, but as the pill needs to override your cycle, we need to accept it’s an artificial situation,” she said.
When it comes to weighing side effects and risks, that should be a consultative approach between doctor and patient, France said.
“When I’m prescribing the pill I say stay on it for three months as it takes a while for your body to adjust,” she explained, as initial side effects will often wane during this period.
That said, Dr France said that a good GP “should be led by the patient because individual experiences are very idiosyncratic.
“If your breasts are a bit bigger than you’d like them to be, but your cramps are gone, your mood is good and your skin is under control, sticking with the pill might be worth it,” she said.
However, if your side effects are “life interfering” France said that ultimately, it’s a GPs job is to supply options.
Related: Hormonal Birth Control For Men Could Be in Our Future
*Is known to POPSUGAR Australia but has requested to remain anonymous.


